The Ultimate Guide to PDPM
Need help navigating all the Patient Driven Payment Model (PDPM) talk out there? We are here to guide the way! Mark has repeatedly combed through CMS Updates for PDPM info and penned previous summaries you may have seen on our old website. Once again, he’s taken the time to go through all the information out there and create a new edition as our PDPM Final Review, so it’s time to tear up the previous summaries and then read or download this new one to understand the upcoming regulatory changes…
UNDERSTANDING THE IMPACT OF THE
PATIENT DRIVEN PAYMENT MODEL
Seagrove Rehab Partners • PDPM Final Review
Prepared by: Mark McDavid, OTR, RAC-CT, CHC
Payment Model Background and Purpose of this Final Review
The Centers for Medicare and Medicaid Services (CMS) introduced the Patient Driven Payment Model (PDPM) in the FY 2019 Proposed and Final Rule process in 2018. In 2019, CMS has further revised and finalized the version of PDPM that will go into effect October 1, 2019. PDPM was originally introduced in Proposed Rule CMS-1696-P, was further modified in CMS-1696-F, CMS-1718-P, and finalized in CMS-1718-F published on August 7, 2019. This article will focus on PDPM and its structure as it is currently understood. The Proposed Rule that introduced PDPM will be referred to as CMS-1696-P and the Final Rule will be referred to as CMS-1696-F. The subsequent proposed and final rules in 2019 updated the model and will be referred to as CMS-1718-F and CMS-1718-P respectively. The following links will take you to the Federal Register where you can download the full version of these documents:
Proposed Rule CMS-1696-P: https://federalregister.gov/d/2018-09015
Final Rule CMS 1696-F: https://federalregister.gov/d/2018-16570
Proposed Rule CMS-1718-P:
https://www.govinfo.gov/content/pkg/FR-2019-04-25/pdf/2019-08108.pdf
Final Rule CMS-1718-F: https://www.govinfo.gov/content/pkg/FR-2019-08-07/pdf/2019-16485.pdf
The New Structure
Over the years, Medicare, MedPac, Congress, and various other stakeholder groups have been pushing to move the payment system away from counting therapy minutes to instead reimbursing SNFs based on patient characteristics and/or patient outcomes. The new PDPM will pay for SNF PPS-care based on patient characteristics and not a volume of services provided. The current RUGs-IV system is a case-mix index-maximizing system; as patients qualify for various RUGs (of the 66 RUGs available), then the system automatically assigns the highest paying RUG for each patient’s reimbursement. This is almost always a Rehab RUG (over 90 percent of SNF PPS days were reimbursed via one of the Rehab RUGs per CMS-1696-P). In the new PDPM, case-mix indexing will still play a role, but there are several different components that will contribute to the reimbursement that will ultimately equal the patient’s daily rate, or per diem. They are: Physical Therapy (PT) component, Occupational Therapy (OT) component, Speech-Language Pathologist (SLP) component, Nursing component, Non-Therapy Ancillary component, and the Non Case-Mix component. The first five of which will be case-mix adjusted based on patient characteristics, and the last will be a flat rate.
Components 1 and 2: PT and OT Case-mix Classification
While PT and OT will be separate components, their case-mix adjustment will be calculated together. There will be two patient characteristics used to determine the PT and OT case-mix classification. They are Clinical Category and Function Score. This process starts by using the primary clinical reason for the patient’s skilled stay to then place that patient into one of four clinical categories. These four categories were created when CMS reduced a set of 10 inpatient clinical categories that they believe capture the range of general resident types potentially found in a SNF. Table 14 from CMS-1696-F outlines those 10 categories:
These 10 categories were further paired down to 4 categories. These will be the 4 Clinical Categories driving the PT and OT case-mix classification:
This clinical category would be determined by the ICD-10-CM code reported in the new MDS item, I0020B. A review of ICD-10-CM mapping to clinical categories (https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/Therapyresearch) will show that in some cases one ICD-10-CM will map to more than one clinical category. The multiple categories are due, in part, to the fact that resident needs will differ depending on whether or not the resident received surgical intervention while in the hospital immediately preceding this SNF stay. Typically, patients who have had surgery in the immediately preceding hospital stay will require extensive post-surgical nursing or rehabilitation care in the SNF. If the patient did not receive a surgical procedure in the immediately preceding hospital stay, then the resulting clinical category will be a non-surgical one. Here is the example given in CMS-1696-P (pages 81-82):
“For example, certain wedge compression fractures that were treated with an invasive surgical procedure such as a fusion during the prior inpatient stay would be categorized as Major Joint Replacement or Spinal Surgery, but if these cases were not treated with a surgical procedure they would be categorized as Non-Surgical Orthopedic/Musculoskeletal. For residents who received a related surgical procedure during the prior inpatient stay, a provider would need to indicate the type of surgical procedure performed for the resident to be appropriately classified under PDPM.”
In order to capture the inpatient surgical procedure, CMS is modifying section J2000 on the MDS. In section J2000 there will be sub-items that will allow providers to report if a surgical procedure occurred during the preceding hospital stay. This will be completed through a checkbox-style mechanism at J2300-J5000.
The next step in determining the PT and OT component case-mix score is to determine the patient’s Function Score. Currently in the RUGs system, CMS uses Section G: Functional Status (or the ADL score section of the MDS) to determine the patient’s functional score. In the new PDPM, CMS has finalized the use of Section GG: Functional Abilities and Goals data to determine the Function Score. Thus, the Function Score will be determined by four late loss ADLs and two early loss ADLs. Specifically, that includes two bed mobility items, three transfer items, one eating item, one toileting item, one oral hygiene item, and two walking items. These were chosen as they are highly predictive of PT and OT costs per day. Tables 16, 17, and 18 of CMS-1696-F graphically show how these items will help produce the Function Score:
The scores for each of the Section GG items above will be added together to get a Total Function Score. This score will be used in Table 21 to further place the patient into the appropriate Case-mix Classification Group. CMS noted that, over time, some Section GG items may be retired and replaced by more relevant, or predictive, items to determine the function score.
Taking 1) Primary clinical reason for SNF stay and 2) Function Score into account, we can now classify a patient into a PT and OT Case-Mix Classification Group. Table 21 graphically shows the breakdown of each PT and OT Case-mix Classification Group:
Component 3: SLP Case-mix Classification
Speech Language Pathology case-mix classification will follow the same methodology as the PT and OT classification. Initially, it will be determined if the primary clinical reason for the SNF stay is either “Acute Neurologic” or “Non-Neurologic”. A quick review of Table 14 above shows that “Acute Neurologic” has its own category and “Non-Neurologic” would be comprised of the 9 remaining categories.
The second characteristic to be identified for the SLP Case-mix Classification is the presence of a swallowing disorder or mechanically altered diet. It is noted that there is increased provider cost for residents with either a mechanically altered diet or a swallowing disorder. And a further increase in cost if the resident has both. Therefore, “both”, “either”, or “neither” are used as it relates to swallowing disorder and mechanically altered diet when determining the SLP Case-mix Classification. These would be identified by responses to K0100A-D, K0100Z, (swallowing disorder) and K0510C2 (mechanically-altered diet) on the MDS.
The third characteristic to be identified for the SLP Case-mix Classification is cognitive status or whether or not the resident had a SLP-related comorbidity present. Table 22 shows the SLP-related Comorbidities:
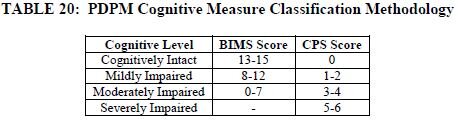
CMS has finalized the use the Cognitive Functional Scale which is a combination of the Brief Interview for Mental Status (BIMS) and Cognitive Performance Scale (CPS) to identify cognitive status for the SLP Case-mix Classification. Table 20 graphically shows how cognition level is chosen using these two tools:
Finally, CMS was able to decrease the number of SLP Case-mix Classification Groups from 18 originally proposed to 12 for PDPM purposes. Table 23 shows the breakdown of how SLP Case-mix Classification Groups will be assigned:
Component 4: Nursing Case-Mix Classification
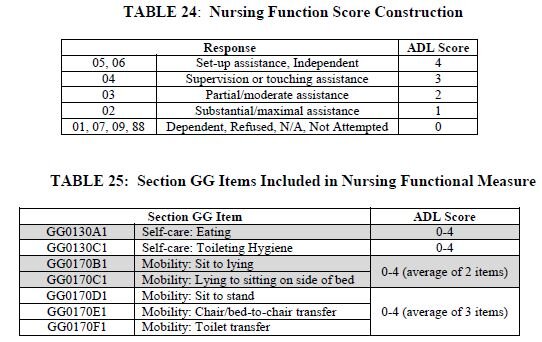
CMS has finalized that the Nursing Case-Mix Classification will be identified based on a modified traditional RUG-IV methodology decreasing the possible RUGs from 43 to 25. In the traditional RUG-IV nursing RUG methodology, the ADL score was derived from Section G of the MDS. Under PDPM, Section GG will be used to determine a Function Score as outlined below in tables 24 and 25:
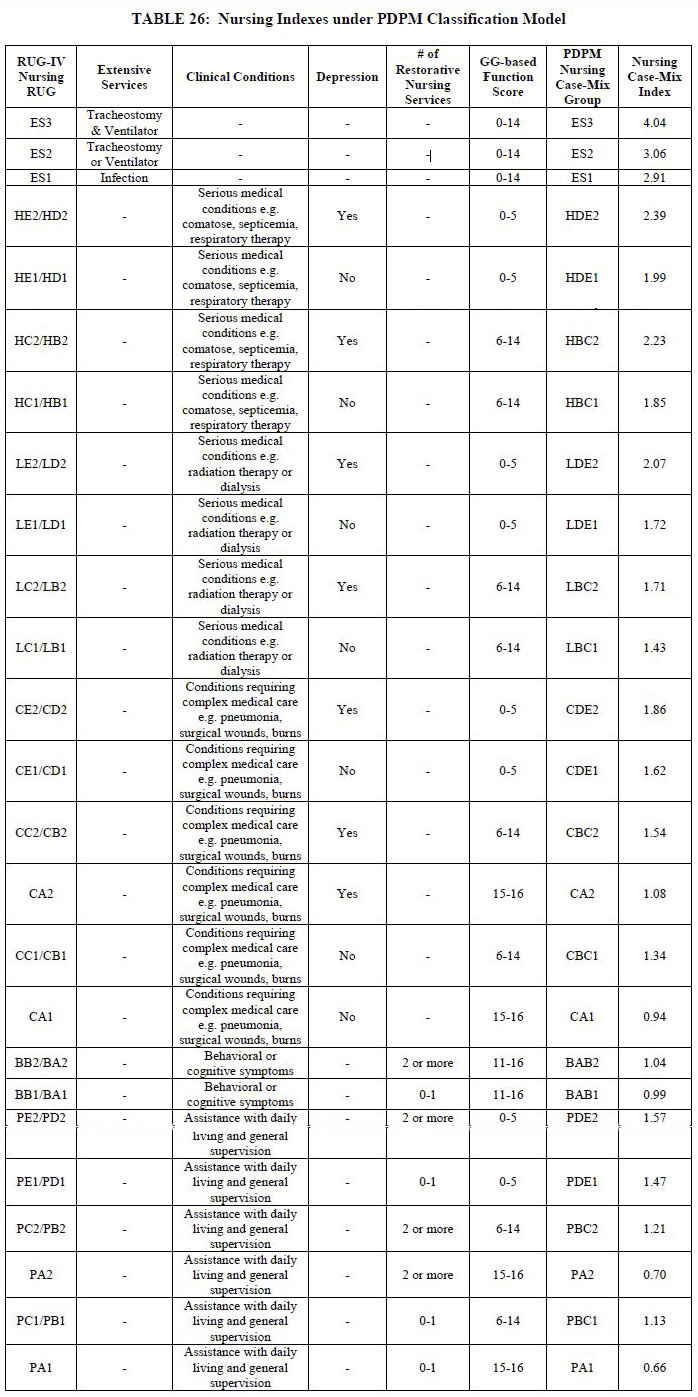
Decreasing the number of RUG options from 43 to 25 was accomplished by collapsing case-mix groups that had contiguous ADL scores when those RUGs were defined by similar clinical traits. Table 26 outlines which RUGs were collapsed and identifies the Nursing case-mix index score:
HIV/AIDS ADD-ON
CMS explained that there was a significant increase in nursing cost to provide care for residents with HIV/AIDS. To compensate facilities for caring for these residents, CMS proposes an 18% increase in the nursing component. This increase would be applied based on the presence of ICD-10-CM code B20 on the SNF claim.
Component 5: Non-Therapy Ancillary
Non-Therapy Ancillary (NTA) scoring is fairly straight forward. Using Table 27 as a reference, if the resident has the condition/extensive service on the left column from the noted source location, then sum the points identified on the right together to get the total NTA score:
Based on the NTA scores summed from the conditions/extensive services on Table 27, Table 28 reflects the NTA Case-Mix Classification Groups:
Component 6: Non Case-Mix Component
The final piece of the total per diem is the non case-mix component. This flat-rate component (that is not case-mix adjusted) is for covering room and board, capital expenses, and administrative overhead.
Combining all 6 components above (PT, OT, SLP, Nursing, NTA, Non Case-Mix) will result in the base daily rate for that patient. Multiplying each component’s base rate by its respective case-mix index will return the facility’s daily base rate for that specific resident upon admission. A portion of the final facility rate will be multiplied by the Wage Index in order to achieve the facility’s final daily rate. As will be discussed below, the Variable Per Diem Adjustment Factor comes in play with PT, OT and the NTA components. These components will be decreased at various intervals during the resident’s stay.
Variable Per Diem Adjustment Factors
Discussed in CMS-1696-P, and finalized in CMS-1696-F, is Medicare’s discovery of decreasing costs of PT, OT, and NTA the longer the resident stays in the facility. This discussion can be found throughout the CMS-1696-P document. Due to the decreasing costs during a resident stay, CMS finalized the Variable Per Diem Adjustment Factor.
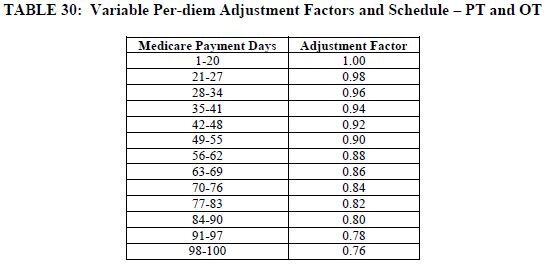
For PT and OT, the facility will be reimbursed the full base rate multiplied by the casemix index, for each resident for PPS days 1-20. Then, starting on day 21, a decreasing adjustment factor of 2% every 7 PPS days will be applied.
An example:
Days 1-20: PT base rate x CMI x 1.00 (the adjustment factor) = PT portion of the per diem
Days 21-27: PT base rate x CMI x .98 (the initial adjustment factor) = PT portion of the per diem.
This decrease will continue for both PT and OT every 7 days as outlined in Table 30 until the patient is discharged. It is worth noting that if the resident stayed all 100 days, the PT and OT components would be reimbursed at 76% of their initial rate for days 98-100.
For the NTA, the finalized adjustment factor starts at a multiple of 3 and is reduced to a multiple of 1 on day 4 as outlined below:
Resident Assessment Instrument: MDS Version 3.0 Changes
As CMS is no longer using therapy minutes to determine reimbursement, any changes in a resident’s therapy minutes will no longer impact reimbursement, therefore, CMS has finalized a new MDS Assessment schedule. The new PPS MDS schedule is represented in Table 33:
*Note that the 5-day Scheduled PPS Assessment may also be called the Initial Medicare Assessment.
Interim Payment Assessment (IPA)
In CMS-1696-P, it was proposed to require an IPA assessment in certain situations. Based on comments, CMS has modified the IPA to now be an optional assessment and the rules surrounding the ARD and payment are as follows:
“Because the IPA will be optional and providers can determine their own criteria for when an IPA is completed, we are revising the ARD criteria we proposed. The ARD for the IPA will be the date the facility chooses to complete the assessment relative to the triggering event that causes a facility to choose to complete the IPA. Payment based on the IPA will begin the same day as the ARD. The IPA will not be susceptible to assessment penalties, given the optional nature of the assessment. We reiterate that we expect facilities to complete IPAs as they deem necessary to address clinical changes throughout a SNF stay and that the removal of the requirement to complete these assessments does not in any way negate the need to provide excellent skilled nursing and rehabilitative care and continually monitor and document patient status.”
CMS has also finalized a change in the rules governing when a PPS Discharge Assessment is to be completed and the Assessment’s Item Set. Currently, the PPS Discharge Assessment is completed when a patient is discharged from Part A and continues to stay in the facility. Under PDPM, CMS will require the completion of the PPS Discharge Assessment for all residents who are discharged from PPS; whether they are actually discharged from the facility or stay long term. Additionally, the Discharge Assessment Item Set will include a modified Section O.
In CMS-1696-P, CMS discusses the comments received in response to the ANPRM publication where stakeholders are concerned about the lack of oversight and monitoring of therapy provisions throughout the stay of the resident. Therefore, CMS has finalized that therapy provisions will be now be monitored throughout the stay by adding Table 35 to Section O on the SNF PPS Discharge Assessment:
The added “Total” items (total individual minutes, total concurrent minutes, total group minutes, total days) are referring to totals throughout the resident’s stay and not just in the 7-day look-back period.
GRACE DAYS
Note: In the current MDS 3.0 RUGs-IV Model, the 5-day assessment, or Initial Medicare Assessment window is days 1-5 with allowable grace days 6-8. CMS has finalized the removal of the label “Grace Days” from the 5-day assessment window. The scheduled assessment window for the 5-day assessment will now be identified as days 1-8 of the PPS stay.
Therapy Provision Policy Changes
Even though we will no longer be using therapy days, modes, and minutes to determine payment, CMS will be reviewing these items to determine how drastically a provider has changed behavior based on the new payment model. It is expected that the majority of therapy provided will be in the individual mode. To that end, CMS is expanding the group limitation to include concurrent therapy as well. In the Final Rule’s version of PDPM, CMS limited group and concurrent treatment provided to a resident to 25% of the minutes provided per discipline across the patient’s stay. This, again, was in response to stakeholder comments where there was concern that a large portion of therapy would now be provided in a group or concurrent setting. Additionally, CMS is going to allow the entire provision of minutes provided in group and concurrent to be recorded on the MDS, which differs from the current RUGs-IV system where the Reimbursable Therapy Minutes are calculated by the group (one fourth) and concurrent (one half) reduction.
Should your therapy department provide more than the allowed 25% of group and concurrent combined per discipline, the provider would receive a non-fatal warning edit on the validation report after submitting an MDS to the QIES ASAP system. This would serve to alert the provider that the modes utilized in the provision of therapy were such that they exceeded the 25% limitation. Note, this would not be a fatal error which indicates that one or more submitted items failed to pass the requirements identified in the MDS. CMS indicates that they will monitor group and concurrent utilization and consider making future proposals to address abuses of this policy or flag providers for additional review.
Also, in CMS-1718-F, CMS has revised the definition of group, it reads as follows:
“...we believe that defining group therapy as therapy provided to groups of 2 to 6 patients at the same time who are performing the same or similar activities would provide therapists with an appropriate amount of flexibility to meet the clinical needs of their patients without compromising the therapist’s ability to manage groups and the patient’s ability to interact effectively and benefit from the group. We expect that therapists will use their professional judgment to determine the most appropriate group size within the bounds of that definition to maximize the benefit to each patient in the group session.”
Interrupted Stay Policy
The interrupted stay policy was finalized in CMS-1696-F. The interrupted stay policy has been finalized to relieve any incentive for providers to discharge a resident with the intent of bringing them back into the facility in a few days in order to reset the Variable Per Diem Adjustment Factors. In the interrupted stay policy, a resident’s PPS calendar will resume with the next PPS day if the resident returns to the facility within 3 midnights (the midnight of the day of discharge counts as one of these three). In cases where the resident returns within this timeframe, there would be no new 5-day Assessment, nor would the Variable Per Diem Adjustment Factor be reset. The resident would return and the payment schedule would continue on the next PPS day continuing with the Variable Per Diem Adjustment Factors in place. This only applies if the resident is out of the facility for less than 3 days. If the resident returns on day 4 or later or is sent to a different facility, then the Variable Per Diem Adjustment Factors are to be reset to day 1 and a 5-day assessment would be required.
A PDPM Example
In an effort to help make the finalized PDPM clearer, let’s take a look at an example of how the per diem will be calculated under the PDPM: Mr. B is a hip replacement patient and has a PT and OT Case-Mix Group of TB, SLP Case-Mix Group of SA, Nursing PDPM Case-Mix Group of CDE2, NTA of NE, and a flat non case-mix rate. The following calculations determine the facility’s per diem covering Days 1-3 for Mr. B’s care.
Due to the Variable Per Diem Adjustment Factors, the NTA changes on day 4 and is constant throughout the rest of the stay. The PT/OT Component decreases by 2% every seven days beginning on day 21. These adjusted rates for our example patient, Mr. B, are listed below:
For Days 4-20, the NTA is 2/3 less:
Urban - $565.35 per day
Rural - $584.25 per day
Starting on Day 21, the PT and OT Components decrease by 2% every 7 days. This results in the following per diem for days 21-27:
Urban - $561.54 per day
Rural - $579.94 per day
Closing Note
As you can see, the PDPM is a vast change from the current RUGs-IV system. It will have large implications for all types of long-term care providers. The review you have just read comprises our thoughts after studying this new concept and leading PDPM presentations dozens of times over the last year and a half. PDPM is something that we, as an industry, are discussing in order to successfully navigate these changing regulations. As we move forward, we will continue to stay abreast of changes. If you are not already a regular client, visit our website to sign up for our update mailing list (seagroverehab.com), or you can follow our Facebook page (facebook.com/seagroverehab). If your company would like a PDPM training or to discuss your current PDPM process, please call (850-532-1334) or e-mail (mark@seagroverehab.com). Also, be on the lookout for any presenting that Mark is doing over the coming months if you attend any therapy-related conferences; he is a regular presenter at annual conferences such as the American Association of Nurse Assessment Coordinators and the National Association of Rehab Providers and Agencies. In addition, he may be speaking at other state and national association meetings near you.
In the meantime, should you or someone in your facility have questions about the new model, please feel free to reach out to us. We welcome the opportunity to create a partnership between our teams.
Mark McDavid, OTR, RAC-CT, CHC
mark@seagroverehab.com
850-532-1334